Yoga and the Vagus Nerve
Emerging Research and a Grounding Practice

Article At A Glance
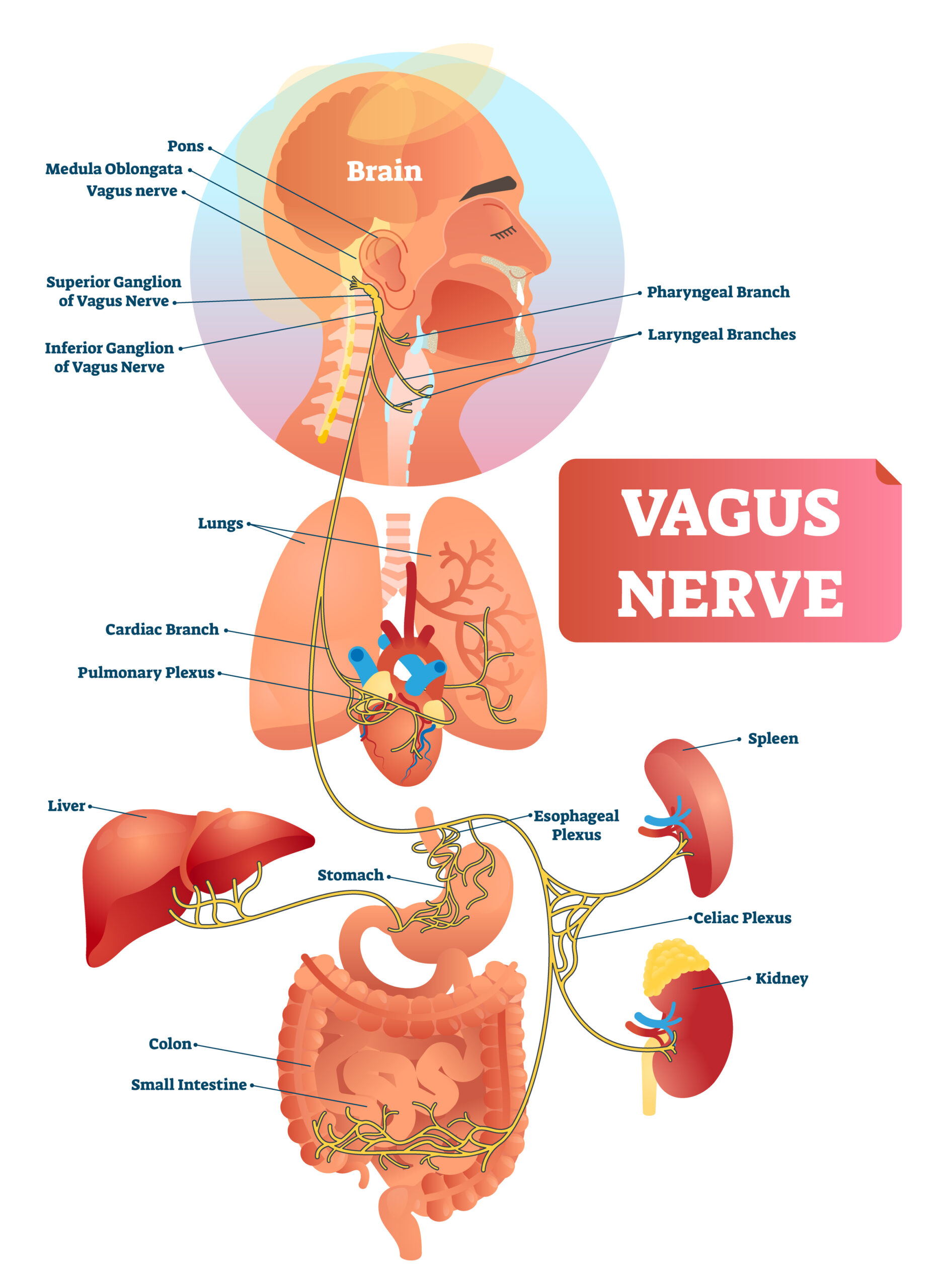
The vagus nerve is the longest of 12 cranial nerves in the autonomic nervous system. The word vagus in Latin means “wanderer,” aptly named because the vagus nerve spans from the brainstem to the colon with branches that innervate the heart, lungs, liver, spleen, and pancreas. This nerve can be thought of as a superhighway that connects the brain to the body, providing anatomical support for the mind-body connection we talk so much about in yoga.
The Vagus Nerve’s Central Role in Stress and Rest
About 80 percent of vagus nerve fibers are sensory, meaning they communicate messages from the body to the central nervous system. In other words, the vagus nerve creates a pathway for yogic postures or breathing techniques felt in the body to reach and calm the brain. And although the vagus nerve plays a role in regulating both the sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) nervous systems, it provides 75 percent of all parasympathetic outflow, making it particularly important in initiating the body’s relaxation response. As part of the parasympathetic response, the vagus nerve also plays a key role in regulating heart rate, blood pressure, digestion, sweating, and breathing.
The Vagus Nerve, Emotional Resilience, and Trauma
In addition to the vagus nerve’s role in the regulation of the autonomic nervous system, you may have heard about its ability to shape our emotional resilience and social connectivity. The rationale behind this thinking comes from Stephen Porges’ polyvagal theory (PVT) (1). Proposed in 1994, the polyvagal theory posits the vagal nerve plays a central role in what Porges outlined as a third division of the autonomic nervous system—a “social engagement system,” which regulates our innate ability to find meaning and connectivity through social relationships but can be disrupted by trauma.

In many ways, polyvagal theory was a landmark idea that brought conversations on trauma’s role in shaping overall health to the attention of yoga teachers, mental health professionals, and somatic-based therapists. It also led to a growing sense of fascination with the vagus nerve among these communities. But how much of the vagus nerve’s role in emotional resilience and social connectivity is evidence-based?
In short, polyvagal theory is fascinating and complex, but it remains a theory with much more research needed to support its claims to help trauma survivors. Without getting too deep into the weeds of the vagus nerve’s physiology, the polyvagal theory is a divergence from traditionally accepted views of the nervous system and is supported by theories that have been widely disputed by evolutionary biologists. This is not to say that certain aspects of polyvagal theory can’t help to heal trauma. But it can do harm if yoga teachers overstep their professional boundaries by making claims to heal trauma through teaching classes or workshops to tone the vagus nerve. Instead, when working with trauma survivors, it’s important for yoga teachers to stay within their scope of practice and refer to licensed mental health practitioners when appropriate.
Heart-Rate Variability and Vagal Tone Research
Polyvagal theory emphasizes vagal tone as a marker of emotional resilience, linking a higher vagal tone to a greater ability to bounce back from stressful life events. Because vagal tone is too invasive to measure, heart-rate variability has been used as an indirect method of understanding vagal tone. However, a study published in 2021 that measured heart-rate variability and vagal activity in rats found there was no correlation between the two (2). Although measuring and understanding heart-rate variability is still of value to understanding the risk of certain health conditions such as diabetes, hypertension, and heart failure, the authors say these results highlight a critical need for reinterpretation of the link between heart-rate variability and vagal tone.
Promising Research on Vagus Nerve Stimulation
Although research supporting polyvagal theory and heart-rate variability to measure vagal tone remain limited, there is promising evidence to support the health benefits of vagus nerve stimulation (VNS). This typically involves surgery performed by a neurosurgeon to implant a small device similar to a pacemaker which sends electrical signals to the brain via the vagus nerve. Clinical use of vagus nerve stimulation has shown clear benefits in treating various health conditions, including drug-resistant epilepsy and depression (3). Vagus nerve stimulation has also been shown to have anti-inflammatory effects, leading to its promise in treating conditions associated with chronic inflammation, such as diabetes and rheumatoid arthritis (3).
The exact mechanism for how vagal nerve stimulation works remains understudied. A 2014 review article in Current Behavioral Neuroscience Reports speculates the success of vagal nerve stimulation may be due to the vagus nerve’s potential role in mediating the relationship between depression, inflammation, metabolic syndrome, and heart disease (4). Despite these promising health benefits, vagus nerve stimulation is invasive and is not suitable for all people, including those with ulcers, asthma, heart arrhythmias, or dysautonomia (abnormal functioning of the autonomic nervous system). Are there more accessible ways to stimulate the vagus nerve? This is where yoga may come into play.
Research on Yoga and the Vagus Nerve
Like many subjects surrounding the vagus nerve, research on yoga and the vagus nerve remains in its infancy. This is especially true as vagal tone is nearly impossible to measure. A 2021 randomized control trial published in the Journal of Alternative and Complementary Medicine showed that compared to a control group who did not participate in yoga, the group randomized to participate in 12 weeks of yoga therapy had significant improvements in a number of markers of metabolic risk, including heart-rate variability (5). As described above, heart-rate variability may not be a perfect measurement of vagal tone, but it may be associated with other health benefits.
So, does practicing yoga truly impact the health of the vagus nerve? More research is needed to say for sure. But what we do know is that other aspects of yoga and movement may help with emotional resilience, nervous system regulation, and overall health. And although the vagus nerve is clearly important, yoga’s impact on health is more complex than its effect on a single nerve.
A Yoga Practice to Target the Vagus Nerve
Can yoga stimulate the vagus nerve? We’ll need more research to find out. But doing postures and practices meant to target the vagus nerve certainly can’t hurt if done mindfully and with the intention of activating the parasympathetic nervous system. Since the vagus nerve travels through the neck, heart, lungs, diaphragm, and abdominal organs, we can practice the following sequence with the vagus nerve in mind. Notice how these activities feel and whether they leave you feeling calmer than when you began the practice. Since rest and relaxation can be individual experiences, take what works for you and leave out what doesn’t.
Diaphragmatic Breathing for the Vagus Nerve
- Begin by coming into a comfortable seat that you can sustain for several minutes.
- Invite your body to ground, imagining roots traveling down from where your body touches the yoga mat into the earth.
- If it feels comfortable to do so, close your eyes or soften your gaze. Start to tune into your natural pattern of breathing, noticing the pace, depth, and length of each inhalation and exhalation.
- Place both hands on your belly and invite your breath to inflate the space around your navel with each inhalation and soften this area with each exhalation.
- Gradually, invite the pace of your breathing to slow down. If it feels helpful to do so, begin to pace your breath, inhaling to a count of four and exhaling to a count of four. After four rounds of breath, begin to lengthen your exhalation, now inhaling for four and exhaling for six.
- Continue this long, slow diaphragmatic breathing for up to 10 more rounds. When you feel complete, return to your natural rhythm of breathing.
Self-Massage for Your Neck
- Flutter open your eyes, adjust your legs for comfort if needed, and return to a seat.
- Take the palm of your right hand to the left side of your neck and begin to gently massage this space. Let the movement of your hand be intuitive, applying only as much pressure as needed to invite a gentle sense of ease. As you massage the left side of your neck, tip your chin down to the right and slowly nod and shake your head to deepen the release. Continue for about 10 breaths, then switch to the second side.
- After massaging both sides of the neck, take both palms to the front of your neck and, very gently, paw the space on either side of the throat. If it feels good, tip your chin slightly upward. After a few breaths, release your hands and return your chin to a neutral position.
Supported Sphinx Pose (Salamba Ardha Bhujangasana)
- Slowly move to your belly, transitioning in any way that feels comfortable for you. Have a bolster, blanket, and/or yoga blocks within reaching distance.
- Come into Sphinx Pose (Salamba Ardha Bhujangasana) by extending your legs behind you and propping yourself up on your forearms with your elbows stacked under your shoulders. To invite a greater sense of ease, you can place a bolster or rolled-up blanket horizontally across your mat so it supports your armpits, upper arms, and chest.
- Gently drop your chin to your chest, perhaps propping your forehead on your bolster or supporting your forehead with stacked yoga blocks.
- Close your eyes and breathe into your belly. Notice how it feels to softly inflate and deflate the space around your navel as you breathe into the earth.
- Stay in this supported shape for 2 to 5 minutes, then slowly transition back to a comfortable seat.
Humming Breath (Bhramari Pranayama)
- Coming back to an upright seat, notice your breath once again. To begin Humming Breath, close your eyes and begin humming with each exhalation, perhaps imagining the sound of a bumblebee.
- Continue humming for about ten rounds of breath. Notice if varying the pitch shifts any feeling in the body or mind.
- When you’ve completed about ten rounds, return to a natural breath and open your eyes.
Also, read...
Do Yoga and Meditation Reduce Health-Care Utilization? What Studies Say
Jun 30 – By: B Grace Bullock, PhD, E-RYT 500
How Exercise Might Help Brain and Nervous System Health
Feb 20 – Nina Zolotow, RYT 500
Can Yoga Help Curb Chronic Inflammation? What the Research Says
Feb 07 – Ram Rao, Ph.D.
Related courses
Breath as Medicine: Yogic Breathing for Vital Aging
With Doug Keller
Yoga and Myofascial Release: Releasing Chronic Tension with the Bodymind Ballwork Method
With Ellen Saltonstall

Lacey Ramirez writes for YogaUOnline and is an RYT-500 & ERYT-200 yoga teacher, global health researcher, and writer based in St. Louis. Through her work, she seeks to make yoga accessible, inclusive, and equitable.
Lacey discovered yoga as a tool for centering during her years as a competitive runner. Since then, yoga has served as a way to connect with her body throughout her experience of pregnancy and parenthood. She teaches because she hopes others can use this sacred practice for calming, healing, and transformation.
As a yoga teacher, Lacey specializes in teaching restorative, Yin, prenatal, and trauma-informed Vinyasa yoga. She has also completed birth doula and prenatal/postnatal barre certifications and trainings. Additionally, she holds a Masters of Science in Global Health and Population from Harvard T.H. Chan School of Public Health. To learn more and connect, visit her website laceyramirez.com
References
(1) Porges, S. W. (2007). The polyvagal perspective. Biol Psychol, 74(2), 116-43. https://doi.org/10.1016/j.biopsycho.2006.06.009
(2) Marmerstein, J. T., McCallum, G. A. & Durand, D. M. Direct measurement of vagal tone in rats does not show correlation to HRV. Sci Rep, 11, 1210 (2021). https://doi.org/10.1038/s41598-020-79808-8
(3) Johnson, R. L., & Wilson, C. G. (2018). A review of vagus nerve stimulation as a therapeutic intervention. J Inflamm Res, 16(11), 203-213. https://doi.org/10.2147/JIR.S163248
(4) Howland, R. H. (2014). Vagus nerve stimulation. Curr Behav Neurosci Rep, 1(2), 64-73. https://doi.org/10.1007/s40473-014-0010-5
(5) Danasegaran, M., Pal, G. K., Sahoo, J., Pal, P., Nanda, N., & Renugasundari, M. (2021). Effects of 12 weeks practice of yoga on heart rate variability in males with type 2 diabetes receiving oral antidiabetic drugs: A randomized control trial. Journal of Alternative and Complementary Medicine, 27(12), 1105–1115. https://doi.org/10.1089/acm.2020.0489
Recent articles
Change Your Perspective of Pelvic Tilting: How the Transversus Abdominis Can Help
Jul 08 – Olga Kabel C-IAYT
Warrior I Pose: 5 Strengthening Variations
Jul 02 – Bridget Frederick, eRYT 500
4 Ways to Practice Locust Pose
Jun 30 – Baxter Bell, MD, eRYT 500, C-IAYT
Categories
Upcoming courses
Breath as Medicine: Yogic Breathing for Vital Aging
With Doug Keller
Yoga and Myofascial Release: Releasing Chronic Tension with the Bodymind Ballwork Method
With Ellen Saltonstall
JOIN NOW!
Recent articles
Almost there...
Sorry, we couldn't find anything...
Pose Library
Change Your Perspective of Pelvic Tilting: How the Transversus Abdominis Can Help
“Tuck your tailbone under” or “lengthen your tailbone” have long been among the most…
Jul 08 – Olga Kabel C-IAYT
Yoga Practice Tips
Warrior I Pose: 5 Strengthening Variations
Warrior I Pose (Virabhadrasana I) is an excellent pose for strengthening your whole back…
Jul 02 – Bridget Frederick, eRYT 500
Pose Library
4 Ways to Practice Locust Pose
Locust Pose (Salabhasana) is a simple backbend that strengthens the entire back of your…
Jun 30 – Baxter Bell, MD, eRYT 500, C-IAYT









